Beyond antibodies, the immune response to coronavirus is complicated
Ultimately, the only way for societies to return to some semblance of normal in the wake of the current pandemic is to reach a state called herd immunity. This is where a large-enough percentage of the population has acquired immunity to SARS-CoV-2—either through infection or a vaccine—that most people exposed to the virus are already immune to it. This will mean that the infection rate will slow and eventually fizzle out, protecting society as a whole.
Given that this is our ultimate goal, we need to understand how the immune system responds to this virus. Most of what we know is based on a combination of what we know about other coronavirus that infect humans and the antibody response to SARS-CoV-2. But now, data is coming in on the response of T-cells, and it indicates that their response is more complex: longer-lasting, broadly based, and including an overlap with the response to prior coronavirus infections. What this means for the prospect of long-lasting protection remains unclear.
What we know now
SARS-CoV-2 is one of seven coronaviruses known to infect humans. Some of these, like SARS and MERS, have only made the jump to humans recently. While more lethal than SARS-CoV-2, we are fortunate that they spread among humans less efficiently. These viruses seem to provoke a long-lasting immune response following infections. That’s a sharp contrast to the four coronaviruses that circulate widely with humans, causing cold-like symptoms. These viruses induce an immunity that seems to last less than a year.
We don’t know much about the immune response to SARS-CoV-2 yet. By tracking the production of antibodies, it’s clear that many of those infected do have a robust immune response, but “many” is far from “all”—there’s a lot of variability in the level of response. That variability is associated with a large difference in the severity of COVID-19 among patients. One area of concern is that the antibody response to SARS-CoV-2 appears to decline rapidly.
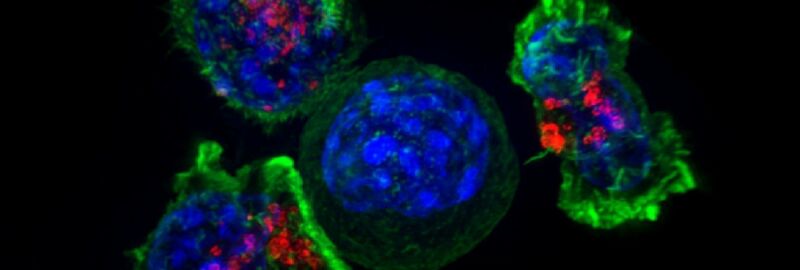
The antibody response, however, is only one part of the immune system’s defense against a pathogen. Antibodies typically recognize the proteins that reside on the surface of a virus, since those are the ones that the cells that make antibodies are exposed to. But a second group of cells, called T-cells, have a different way of recognizing pathogens. T-cells rely on a system used by all cells, which takes small pieces of the proteins they are making and presents them on the cell surface. Because of how the system works, it has the potential to recognize more of the proteins made by a virus—not just the ones on its surface.
(Some immune cells that swallow pathogens also put protein fragments on their surface in the same way.)
Once there, any T-cells that recognize these small pieces of protein as foreign can mount a variety of responses, from activating their fellow immune cells to killing the cell that is making foreign proteins. Studying the T-cell response is much more challenging, since it’s based on cells, rather than antibodies, which are proteins. But such study can be equally critical to long-term immunity.
Studying the Ts
To study the T-cell response, a group of researchers based in Singapore focused on proteins that are either internal to the virus or used only in the cells it infects and thus aren’t a major focus of the antibody response. To check the response to these proteins, the researchers made a set of 15-amino-acid-long protein fragments that, collectively, span the entire length of the protein. They then collected blood cells from people who had recovered from COVID-19, those who recovered from the original SARS, and those who have never been exposed to either virus.
These fragments were pooled and mixed with blood cells to determine whether any T-cells within them reacted to them. By narrowing down the pools, the researchers were able to identify the specific fragment—and thus the specific region of the protein it came from—that T-cells were responding to. The response was registered by checking the level of an immune-signaling molecule produced by T-cells.
One of the potentially reassuring findings was that people who had been exposed to the original SARS virus 17 years earlier still had T-cells that responded to fragments of the virus. This was true even though the antibody response to this virus had generally faded after several years. Less surprisingly, the people who had recently had COVID-19 also had T-cells that responded to fragments of the virus’ proteins.
But there was a striking feature of the SARS and COVID-19 fragments that the T-cells responded to: many of them were identical. While SARS-CoV-1 and -2 are distinct viruses with different evolutionary histories, many of their proteins remain extremely similar. (That’s probably because they continue to perform similar functions, and thus there’s evolutionary pressure against changes.) As a result, several of the fragments that were made based on the SARS-CoV-2 proteins happened to be identical in the equivalent protein of SARS-CoV-1. So a T-cell that recognized one of these fragments could recognize both viruses—even though it came from a patient who had only been exposed to only one.
Surprise!
That sets the stage for the most surprising result of the study. Participants who had never been exposed to either SARS virus also had some T-cells that recognized pieces of SARS-CoV-2 proteins. This wasn’t true for every participant in the unexposed group; only about half of them had these reactive T-cells. But again, it was mostly based on cells that reacted to pieces of protein that were identical between SARS-CoV-2 and viruses that cause the common cold.
Mostly, but not all. There were two exceptions to this—two fragments of protein that didn’t look like the cold virus but provoked a response from T-cells of unexposed participants—and the researchers struggle to explain them. Their only suggestion is that some other pathogen happens at random to have a small section of protein that looks like this. There were also differences among the groups regarding which of the three proteins their T-cells recognize, but the significance of these differences are not clear.
What’s it all mean?
So, does this mean the common cold can potentially protect some of us from COVID-19? There’s no way to know based on these results. Prior exposure to cold-causing coronaviruses seems to induce a response to different proteins than exposure to SARS-CoV-2. And there’s no indication that antibodies to the common cold viruses cross-react to SARS-CoV-2. Would a T-cell based response on its own be enough to ward off the virus? We don’t know.
At the same time, the fact that this response is only present in a subset of the people who have never been exposed could potentially account for some of the differences in the severity of COVID-19 symptoms. There’s obviously a lot more work to be done here.
The importance of T-cell-based immunity is also critical to understanding the issue of the apparently highly variable antibody response as well as the indications that it may fade out rapidly once the SARS-CoV-2 infection is cleared. This study indicates that T-cell responses are consistent and strong in this small population. The parallel work on SARS patients indicates that this response also lasts much longer than the antibody-based immune response. So, if it’s sufficient to provide protection from reinfection, then we might be able to worry less about the erratic antibody response. Again, we don’t know yet.
This could also have implications for the development of vaccines, which tend to focus on the production of neutralizing antibodies.
All of which implies that there’s an urgent need to better understand the T-cell response to SARS-CoV-2. Which is unfortunate, given how challenging studying T-cells is.
Nature, 2020. DOI: 10.1038/s41586-020-2550-z (About DOIs).
https://arstechnica.com/?p=1692480