Face masks don’t even have to work especially well to be effective

Advice on whether or not to use face masks to limit the spread of the pandemic has varied from country to country, even differing by location within countries. These policies have had to balance whether there were sufficient supplies for medical personnel to divert some to the general public. And the whole issue was decided without a clear idea of whether face masks were actually effective against SARS-CoV-2.
But there has been reason to think masks would at least be somewhat effective, based on studies of the spread of droplets of material we expel while coughing or sneezing. And a recent analysis suggested a large group of individual studies collectively pointed to their effectiveness. But that analysis left a large degree of uncertainty about how effective they’d be at the population level and how face mask use would interact with other policy decisions.
The situation left us needing population-level modeling, which a group of UK scientists has now provided. The group’s model indicates that face masks don’t have to be especially effective to slow the spread of SARS-CoV-2—as long as they limit the spread of the virus from infected people, they can limit the pandemic even if they make mask wearers more susceptible to infection. But to really control the pandemic, masks will have to be combined with a lockdown if we want to see the total infected population shrink.
Masks vs. virus
Mask use actually has two different functions. To a degree, it limits the ability of people who are infected to put infectious particles into the environment. And to a potentially different degree, it limits access to two of the primary routes by which those particles can reach new hosts: the mouth and nose. It’s not a complete solution, as a person’s eyes are still uncovered, and the degree of effectiveness will vary based on how many potentially infectious particles are filtered out. Still, even a crude mask is likely to capture many of the largest particles we produce, and those are the ones that will carry the most viruses.
There’s also some uncertainty about the virus’s behavior. We don’t know how much of it is present in a typical droplet expelled by an infected person or how long the virus remains infectious once those particles make it to the environment. There’s also some residual uncertainty about when a person becomes infectious relative to the onset of symptoms. While some of these unanswered questions don’t alter the effectiveness of masks, they can influence how effective policies on mask use are.
To get around these issues, the researchers decided to model a wide range of conditions, some in which the face masks were only slightly effective and others in which they blocked much of the spread of the virus. The authors even ran models in which wearing a face mask was assumed to increase the chances of someone becoming infected by causing people to bring their hands to their faces to adjust the mask’s fit.
To get at all these questions, the researchers relied on two different models. The first was something called a “branching process model” that got at the question of how effective a face mask had to be before it could influence the rate of transmission of SARS-CoV-2, based on how many people were wearing masks. They ran this model with two different base rates of infectivity and looked at how different levels of effectiveness and use changed those rates.
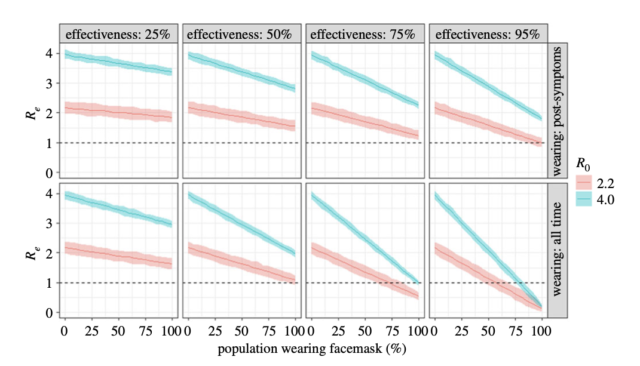
In the graph above, the blue bars represent a high rate of infectivity (each infection results in four additional ones) and the second a more moderate rate (2.2 new infections for every one). Even low levels of use of ineffective masks were able to bring the rate of viral spread down toward a rate of 1, below which the pandemic would gradually stop spreading.
But for the most part, mask use alone isn’t able to get there. If, as in the top row, people start wearing masks after the onset of symptoms, there are no scenarios in which face masks alone are able to stop the pandemic—even if they are 95-percent effective and everyone with symptoms wears them. By contrast, if everyone wears them all the time, even a 75-percent effective mask could possibly bring the rate of new infections down on its own.
More policies
But using face masks isn’t likely to occur in a vacuum; it’s going to be part of a suite of policy solutions implemented in response to the pandemic. So the authors built a second model based on a standard epidemiology approach that divides a population up into pools of susceptible, infected, and recovered people. They layered a fair bit of complexity onto this approach, splitting the population up into mask-wearers and those without, breaking out exposed, asymptomatic, and symptomatic groups and building an exposure process that took into account the formation and spread of virus-containing droplets.
This last piece of the model was essential to considering the role of masks, as they influence both the spread of these droplets into the environment and a susceptible person’s exposure to them. The model also assumes that anyone who reaches the recovered state is immune to further infection—something that has yet to be confirmed.
Running the model with no face mask use and lockdowns in response to high infection levels produces what pretty much every model has seen: a large peak of infection that induces a lockdown, a recovery period in which the lockdown is relaxed, followed by an additional peak. In this model, three individual peaks are seen before sufficient immunity is reached to start slowing further waves of infections.
Assuming a face mask that’s even less effective than cotton cloth is at preventing the spread of droplets, a 50-percent rate of mask use is able to delay further peaks. The second peak, for example, would start at about the same time that the population is already in lockdown under the no-mask-use scenario. At 100-percent face mask use, there’s only a single wave of infections and then the pandemic starts to decline. In this scenario, infections will decline even if face masks are only 50-percent effective. With 95-percent mask use, an N95-level of protection is enough to cause the pandemic to decline.
As mentioned above, the researchers also considered a scenario where wearing masks makes people more susceptible to infection, as they touch their face more often because of the mask’s presence. While mask wearers suffer in this scenario, the population overall still benefits under most conditions in which at least two-thirds of the population is wearing masks. That’s because there are so many fewer infectious particles around that this offsets the increased susceptibility.
Models meet the real world
Right now, we just don’t know enough about SARS-CoV-2 and protective gear to evaluate which of these models best reflects reality. But the models do set some reasonable bounds about what we might aim for. For example, they indicate that masks don’t need to be especially good if we get enough people wearing them and couple their use to other policy initiatives.
A few indications that mask use is working in the real world are starting to crop up. For example, an economics institute in Germany looked at the implementation of mask rules in the city of Jena, comparing it to other areas in Germany. It concluded that the rules reduced the growth of the infection rate by 40 percent. (Note that’s the growth rate, not the overall rate of infection.) A non-peer-reviewed study published by PNAS found that mask use made a difference in China, Italy, and the US, although some of the data isn’t entirely compelling. (Looking specifically at Figure 3A, face mask rules seem to have been put in place after infections were already trending downward.) There’s nothing conclusive yet, but there’s some suggestive evidence, and no signs that face mask use is making matters worse.
Proceedings of the Royal Society A, 2020. DOI: 10.1098/rspa.2020.0376 (About DOIs).
https://arstechnica.com/?p=1683437