In depression treatment trials, placebo effect is growing stronger
Placebos have occupied an increasingly awkward spot in the medical landscape over the last few decades. Even as placebo-controlled trials have become accepted as the gold standard for evidence, we’ve grown to appreciate just how powerful the placebo effect can be. Confusing matters further, a new study has expanded on a previous finding: The placebo effect for antidepressant treatments appears to be growing stronger over time.
Earlier work had shown this was happening with placebo pills. The new study shows that it’s happening with a treatment called transcranial magnetic stimulation. Fortunately, effective treatments appear to be getting better in parallel, so this hasn’t obviously interfered with any results yet.
Stimulating magnets
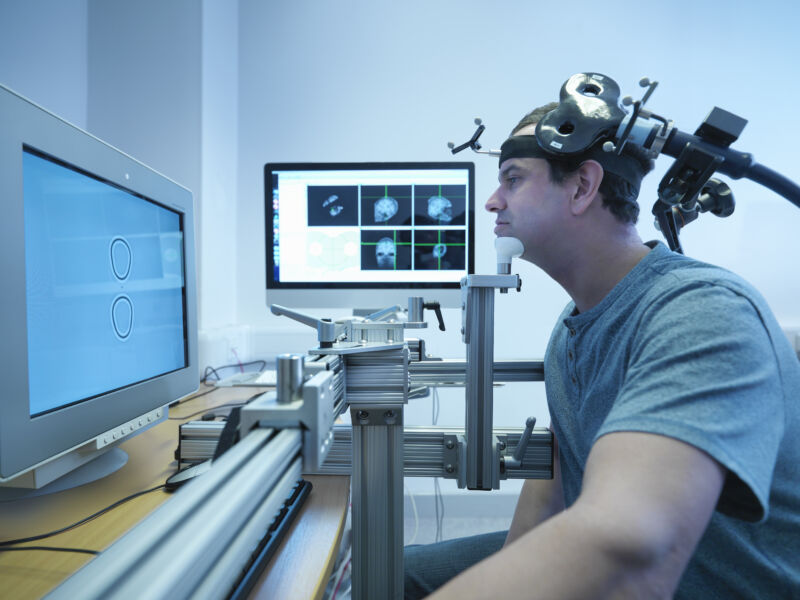
Transcranial magnetic stimulation is fairly straightforward in principle. It’s possible to use magnetic fields to induce currents in many materials. One of the materials where that works is the brain, where neural activity depends on the presence of voltage between a cell and its environment. So, by carefully shaping the magnetic field, it’s possible to influence the activity in specific areas of the brain. Critically, this can be done with equipment placed outside the skull and, so, is quite non-invasive compared to many other interventions.
There are, however, a number of limitations of the technique. It’s challenging to target areas deep in the brain, and it’s somewhat inexact—it’s difficult to target a small enough region that you’re only going to be altering the behavior of neurons involved in a single process. In addition, there are lots of options when you can vary the length, intensity, and number of magnetic pulses you create. Figuring out the combination that will best target and treat a specific disorder requires a lot of work.
Nevertheless, there have been clinical trials for a large array of disorders, one of them being depression. And many of these have had a placebo control; these can involve placing inactive hardware next to the skull or orienting the magnetic fields so that any stimulation occurs is next to the skull, rather than under it.
When it comes to depression, however, placebos have been acting a bit strange over the past few decades: They’ve been getting more potent since at least the 1980s. A number of studies have shown this is the case for pill-based placebos, and a few have hinted that it applies to transcranial magnetic stimulation as well. The new study aims to be a comprehensive meta-analysis that’s large enough to both test whether the improvement really exists, and to figure out if it’s associated with any specific types of study.
Better over time
The researchers started with a pool of over 2,700 individual studies that used transcranial magnetic stimulation to treat depression. After selecting for high-quality clinical trial data that included randomization and blinding, they were left with only 52 trials and a total of 4,500 participants, about half of which received a placebo treatment.
These placebos always involved hardware, but the hardware could be either inoperative or mis-directed. The non-placebo treatments included a variety of different transcranial magnetic stimulation approaches.
Since you can’t really do a placebo control for a placebo, the work simply focused on whether the participants reported improvements in their conditions. And, in fact, the placebos did, pretty consistently, although the actual treatment typically had a larger effect. (Using a measure called the “response magnitude,” the placebo was rated at 24 percent, while the actual treatment hit 38 percent.)
To look into whether things were changing over time, the researchers divided the trials up into two batches, one covering the years between 1999 and 2007, and a second covering 2018 to 2022. The effect of both the placebo and the treatment went up over time. The two, however, went up in parallel, so the change didn’t affect the trial outcomes.
The researchers performed a regression analysis to find out which factors might be influencing these correlations. As expected, this analysis showed a correlation between the placebo effect and the impact of the actual treatment. Trials performed in North and South America also tended to have a larger effect, as did a measurement of the risk of bias in each of the studies.
The placebo is real
That doesn’t mean that the placebo effect isn’t happening here. The researchers estimate that it would take nearly 7,500 new studies showing that there is no placebo effect for it to go away entirely. But it does suggest that at least some of the differences between earlier and later trials may come down to study design. “Over the past 20 years, patient populations, transcranial magnetic stimulation protocols, equipment and technology, sham procedures, trial methodology and execution have all undergone significant shifts,” they note.
And these are some of the things that can potentially influence how people perceive the sham treatment. After all, the placebo effect is largely mediated by the belief that some form of treatment is happening. Transcranial magnetic stimulation, which involves medical staff and some serious-looking equipment placed next to someone’s head, lends itself very readily to that belief. If more effort has been put into making the placebo convincing in recent years, it could easily explain the change we’re seeing.
Unfortunately, details on placebo procedures are often not reported in detail in studies, making it harder to understand which specific changes might be driving this effect.
Nature Mental Health, 2023. DOI: 10.1038/s44220-023-00118-9 (About DOIs).
https://arstechnica.com/?p=1971234