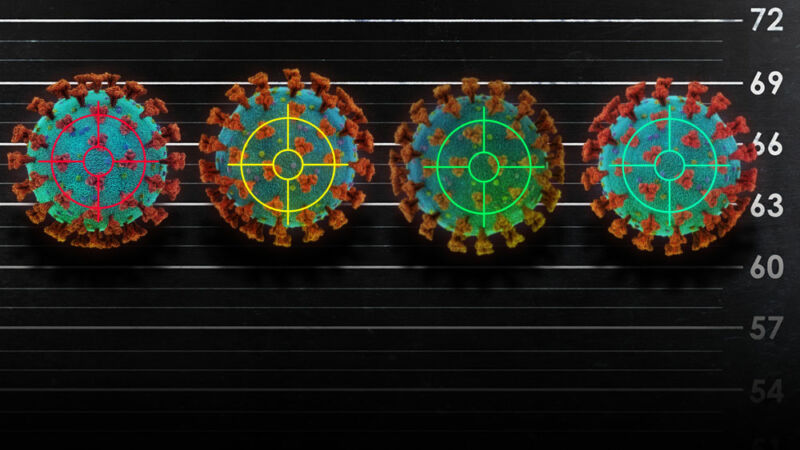
Researchers have now reported data from early (and small) clinical trials of four candidate COVID-19 vaccines.
So far, the data is positive. The vaccines appear to be generally safe, and they spur immune responses against the novel coronavirus, SARS-CoV-2. But whether these immune responses are enough to protect people from infection and disease remains an important unknown.
The four candidates are now headed to larger trials—phase III trials—that will put them to the ultimate test: can they protect people from COVID-19 and end this pandemic?
The challenge
While early trials looking at safety and immune response required dozens or hundreds of volunteers, researchers will now have to recruit tens of thousands. Ideally, volunteers will be in places that still have high levels of SARS-CoV-2 circulating. The more likely it is that volunteers will encounter the virus in their communities, the easier it is to extrapolate if a vaccine is protective. As such, researchers are planning to do a significant amount of testing in the US and other parts of the Americas, which have largely failed at controlling the pandemic.
There has been much debate about the use of “human challenge trials,” in which researchers would give young, healthy volunteers at low risk from COVID-19 an experimental vaccine and then intentionally expose them to SARS-CoV-2 in controlled settings. This could potentially provide a clearer, faster answer on vaccine efficacy. It’s certainly an appealing idea given the catastrophic pandemic—and it’s an idea that has gained traction in recent weeks. An advocacy group called 1Day Sooner has collected the names of more than 30,000 people willing to participate in such a trial, for instance.
But experts remain divided on the idea. The main concern is that there is no “rescue” treatment for COVID-19 that can fully protect a trial volunteer from severe disease and death if an experimental vaccine fails. Though young, healthy people have less risk than older people and those with underlying health conditions, some still suffer severe disease and death from COVID-19—and it’s unclear why. Opponents also note that challenge trials may not be faster or necessary, given the high levels of disease spread in the US and elsewhere.
Though the debate on challenge trials is ongoing, it’s unclear if researchers will end up needing or using them. Meanwhile, traditional phase III trials are now underway—and they have generated plenty of enthusiasm from the public. According to a report this week, more than 138,600 people have signed up through the National Institutes of Health to participate in vaccine testing. If all goes well, we could have data from these trials by the end of the year.
So how do the four top vaccine candidates work, and what do we know about them?
mRNA-1273: Moderna, NIAID
mRNA-1273 is a messenger RNA (mRNA) vaccine made by the biotechnology company Moderna, which was working with the NIH’s National Institute of Allergy and Infectious Diseases (NIAID). The idea behind the mRNA vaccine platform is that it delivers snippets of a target virus’s genetic code—in this case, code in the form of mRNA—into human cells. Those cells can then translate that code into viral protein. From there, the immune system can mount a response to the protein, which can be activated if the target virus ever tries to invade.
In the case of mRNA-1273, researchers used a fatty nanoparticle to package up mRNA that codes for the SARS-CoV-2 spike protein, which is usually found jutting out from SARS-CoV-2 viral particles.
Vaccines using genetic material—RNA or DNA—are new and untested. So far, there are no approved vaccines using this type of platform. It’s unclear if they will be successful here or elsewhere and—if they are—how easy it will be to manufacture such a vaccine on a global scale. (For background on the different types of vaccine platforms, see our vaccine primer.)
On July 14, researchers published results from a phase 1 trial, which primarily looks at safety in a small group of people. The study, appearing in the New England Journal of Medicine, included 45 healthy volunteers between the ages of 18 and 55 and tested three dose levels of the vaccine. That is, there were three groups of 15 people, with each group getting either a low, medium, or high dose of the vaccine (25 micrograms, 100 micrograms, or 250 micrograms dose). Each participant got two shots of their dose, 28 days apart.
The vaccine was generally found to be safe. More than half of the participants had mild to moderate side effects, mainly including fatigue, chills, headache, myalgia, and pain at the injection site. Side effects were more common after the second dose, regardless of the strength, but those who received the two higher-dose vaccinations reported more side effects. Two people (one in the 100-microgram group and the other in the 250-microgram group) had severe skin redness at the site of the injection. Two people in the 250-microgram group experienced lightheadedness and fainted.
All participants produced antibodies against SARS-CoV-2, with antibody levels jumping up after the second shot. Those who got the higher doses had slightly higher levels of antibodies. The researchers compared participant antibody levels to those seen in 41 people who had recovered from a COVID-19 infection. Those vaccinated all had antibodies in the same range as the recovered people.
The researchers also tested specifically for neutralizing antibodies—that is, antibodies that don’t just bind to a virus particle but can completely disable it. Researchers found that the vaccine prompted higher levels of neutralizing antibodies than was seen in most of the people who recovered. For instance, 57 days after the first dose, people in the 100-microgram group had neutralizing antibody titers ranging from 163 to 329, while the range was about 60 to 200 in the patients who had recovered from COVID-19.
Last, the researchers looked at responses from T-cells—which can attack cells infected with virus—and found that the vaccine did generate certain types of T-cell responses against SARS-CoV-2.
Overall, the results are encouraging but not conclusive. Researchers don’t yet know what immune responses or levels of antibodies are necessary to prevent a SARS-CoV-2 infection and/or disease. And, being only six months into the pandemic, it’s unclear how long any such protective immune responses would last.
According to a listing on the NIH’s registry for clinical trials, Moderna plans to begin a phase III trial of mRNA-1273 on July 27. Moderna wants to enroll 30,000 people in the trial, looking at efficacy as well as further safety and immune response data.
AZD1222 (ChAdOx1 nCoV-19): Oxford University, AstraZeneca
On July 20, researchers published results from a phase I/II trial of AZD1222, a candidate vaccine made by researchers at the University of Oxford and the international pharmaceutical company AstraZeneca.
AZD1222 (also called ChAdOx1 nCoV-19) is a viral vector-based vaccine. With this platform, researchers can package bits of a dangerous virus into a far less dangerous virus. The mostly harmless viral parcel then gets delivered to the immune system, which can learn to seek and destroy the dangerous virus based on the smuggled fragments.
In the case of AZD1222, genetic material of the SARS-CoV-2 spike protein is packaged into a weakened type of adenovirus that infects chimpanzees. Human-infecting adenoviruses normally cause mild infections, often considered common colds. The chimpanzee virus, which doesn’t typically infect humans, is made even more harmless by engineering that prevents it from replicating in human cells. In early tests, AZD1222 protected monkeys from developing pneumonia after researchers exposed them to high doses of SARS-CoV-2.
The clinical trial results, published in The Lancet, show that AZD1222 is generally safe and spurred immune responses in humans. The trial involved 1,077 participants (aged 18 to 55), 543 of which were randomly assigned to get AZD1222, and the remaining 534 were given a meningococcal vaccine as a control. Researchers divided the participants into four groups and ran different types of tests on their immune responses. Ten of the participants who received AZD1222 were in a “boost” group that got a second vaccine shot after 28 days. The other participants who received AZD1222 only received one dose.
Mild side effects from AZD1222 were common, including pain, feeling feverish, chills, muscle ache, headache, and malaise. Some participants were preemptively given paracetamol (acetaminophen/Tylenol) to lessen these effects. No serious side effects were reported.
In 127 participants vaccinated with AZD1222, all produced antibodies against SARS-CoV-2. The levels were within the range seen in people who had recovered from COVID-19. The researchers conducted two separate tests to look for neutralizing antibodies in 35 vaccinated participants. In one test, 32 (91 percent) were positive for neutralizing antibodies 28 days after vaccination and, in the other test, 100 percent were positive. The ten participants who got a booster shot all produced neutralizing antibodies, some which were at levels higher than those typically seen in the COVID-19 recovered patients. The researchers also reported that AZD1222 induced T-cell responses.
Researchers have already begun a phase III trial of AZD1222 at sites in Brazil, the UK, and South Africa. They also plan to test the vaccine in the US soon. AstraZeneca said it will use two doses in trials moving forward in order to maximize immune responses.
https://arstechnica.com/?p=1693804

