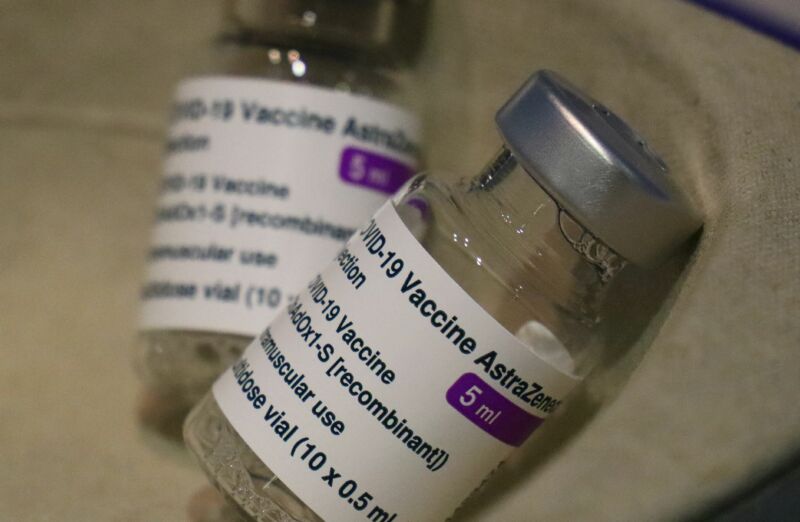
Exceeding expectations, AstraZeneca’s two-dose COVID-19 vaccine appeared highly effective against symptomatic and severe disease in a new late-stage trial conducted partly in the US. The company said it is now seeking emergency use authorization from the Food and Drug Administration. However, the vaccine may still be dogged by doubts.
The Phase III trial conducted in the US, Peru, and Chile found that the vaccine was 79 percent effective at preventing symptomatic disease, the company reported early Monday. Previous trial results suggest efficacy could be as low as 62 percent.
In the new 32,449-person trial, two-thirds of participants were dosed with the vaccine while the remaining third were given a placebo. There were five cases of severe disease in the trial, all in the placebo group. None of the vaccinated participants required hospitalization.
Notably, the company also found no increased risk of blood clotting events or cases of a rare, life-threatening blood clotting event, called CVST, among those vaccinated.
Blood clots
A small number of serious blood clotting events in people recently vaccinated sparked widespread concern in Europe and other countries, where the vaccine is already authorized for use. In the last week or so, more than a dozen countries—including Germany, France, Italy, and Spain—temporarily halted their rollouts of AstraZeneca’s vaccine, which was developed in collaboration with the University of Oxford.
Among the more than 20 million people who have already received the vaccine in the European Union and the United Kingdom, there have been at least 18 reported cases of CVST (cerebral venous sinus thrombosis), in which a clot prevents blood from draining from the brain, leading to a stroke. There were also at least seven other cases of people developing blood clots in multiple blood vessels, a condition called disseminated intravascular coagulation, or DIC. Nine of the CVST and DIC cases resulted in death.
Last week, the World Health Organization and the European Medicines Agency independently reviewed all the data in detail and, in the end, urged countries to quickly resume use of the vaccine. Both agencies concluded that the risks of severe disease and death from COVID-19 clearly outweighed the exceedingly rare risk of blood clotting events.
The WHO and the EMA noted that among the millions of vaccinated people, reports of blood clotting events—which are generally common—were lower than what would have been expected in the general population. They also couldn’t establish whether the vaccine caused the cases of CVST or DIC. But they couldn’t rule out the possibility, either, particularly since most of the cases were in people under the age of 55.
In the EMA’s review, the organizations noted:
Based on pre-COVID figures, it was calculated that less than 1 reported case of DIC might have been expected by 16 March among people under 50 within 14 days of receiving the vaccine, whereas 5 cases had been reported. Similarly, on average 1.35 cases of CVST might have been expected among this age group whereas by the same cut-off date there had been 12. A similar imbalance was not visible in the older population given the vaccine.
Lingering questions
The new trial results didn’t find any cases of CVST, but—if there really is a link—this isn’t surprising based on the extremely low frequency of these events. The trial data included safety data for just about 21,500 vaccinated people, whereas the small number of cases outside of the trial occurred among upward of 20 million vaccinated people.
While there’s the real possibility that the cases are simply a statistical fluke, some researchers hypothesize that the vaccine may—rarely—spark an autoimmune reaction that explains the illnesses, and they have suggested possible treatments along those lines. Other researchers have also noted that a link between the vaccine and blood clotting events is not implausible; COVID-19 itself is linked to blood clotting disorders, and research suggests that the SARS-CoV-2 spike protein can activate immune responses that can lead to clotting.
But it will take much more data to firmly make the connection (if there is one), as well as figure out how such a reaction is sparked by the vaccine, and who might be affected. Like the other authorized COVID-19 vaccines, the AstraZeneca vaccine delivers to cells only the genetic code for the SARS-CoV-2 spike protein, which can train immune responses to target the virus. The vaccine does this using a non-replicating adenovirus as packaging, similar to the Johnson & Johnson vaccine, which was the latest vaccine authorized by the FDA.
For now, eyes will be on the FDA as it reviews the data and decides whether to grant an EUA. The agency is likely to look favorably on the efficacy and safety data of the new trial and see the vaccine as yet another useful tool in the fight against SARS-CoV-2. Still, gaining public support may be a bigger hurdle for the vaccine moving forward. Aside from the blood clotting concerns, the vaccine has experienced stumble after stumble in its clumsy development—from highly publicized trial pauses due to unexplained illnesses and puzzling dosing errors in some participants, to recent data suggesting it may be useless against mild-to-moderate COVID-19 caused by the B.1.351 variant.
https://arstechnica.com/?p=1751215

