Catching malaria in the US is extremely rare, but when it happens, the mosquito-borne parasite can masquerade as another parasite that’s regularly found in the country, leading to a misdiagnosis that has foiled doctors around the world for years. Such was the case this year in Maryland, when the state saw its first locally acquired malaria case in over 40 years, according to a report this week.
The misdiagnosis led the patient to a weeks-long treatment for the wrong infection and held up public health responses to pinpoint and thwart further transmission. To date, the source of the patient’s infection remains a mystery.
As global travel and climate warming expand malaria’s range, awareness of the diagnostic pitfall and better testing will be increasingly needed, the report’s authors suggest. The report was published Thursday in the Centers for Disease Control and Prevention’s Morbidity and Mortality Weekly Report.
Malaria rages in large swaths of the world but was considered eliminated from the US in 1951. Still, there are around 2,000 malaria cases in the US each year, all linked to travel to areas with malaria transmission. The state of Maryland sees around 200 such cases in a typical year.
Then there are years like this one—when there were nine malaria cases that were locally acquired (not linked to travel) in the US: seven in Florida, one in Texas, and one in Maryland. It was the first year in two decades that any locally acquired malaria was found anywhere in the US. The last local cases occurred in 2003 in Palm Beach, Florida.
Yet, the three states’ cases were not linked. The seven cases in Florida clustered in a swampy area near an imported malaria case. The unrelated Texas case was also in the vicinity of an imported case. In Florida and Texas, the cases were caused by the malaria parasite Plasmodium vivax, which spreads in many places around the world, including South and East Asia, the Western Pacific, and South America. In Maryland, the case involved P. falciparum, which causes the deadliest form of malaria and spreads heavily in African countries.
Maryland case
On August 6, a previously healthy Maryland resident showed up at a health facility after seven days of fever, muscle pain, and malaise. The person had no recent international travel but noted taking daily walks near home and having recently been bitten by a tick. Lab tests showed anemia, low blood platelets, and a buildup of bilirubin (which occurs when red blood cells break down). The patient also had parasites in their red blood cells.
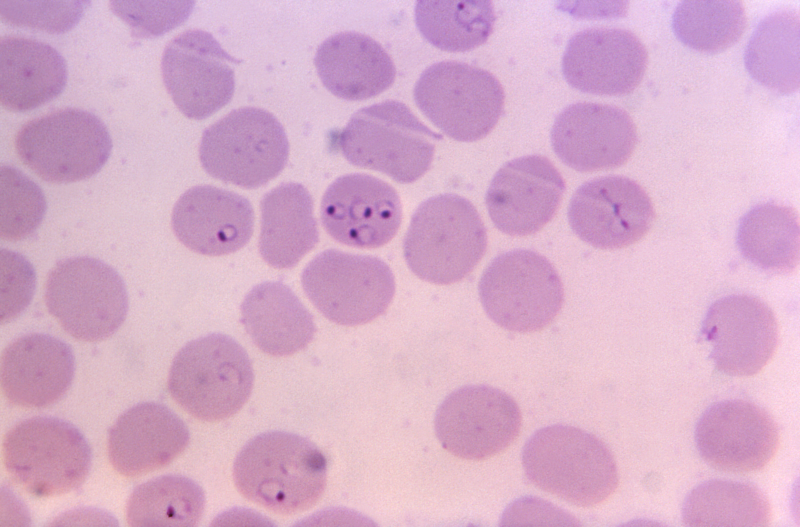
These symptoms and findings match two diseases: malaria and another parasitic infection called babesiosis, which is caused by Babesia parasites and spread in the US by ticks. Given the circumstances, doctors admitted him to a hospital and began treatment for babesiosis.
On August 9, a blood smear report indicated P. falciparum, though. The doctors shared the smear images with the CDC, but the images weren’t clear enough for CDC experts to distinguish whether Babesia or P. falciparum were in the patient’s red blood cells. With special stains and microscopy, both parasites look like little rings inside red blood cells.
https://arstechnica.com/?p=1975941

