
In the US, federal law has severely restricted our ability to study any potential medical properties of cannabis. But, given some limited studies and a lot of anecdotal stories, a number of states have gone ahead and legalized medical marijuana. This has allowed some population-level studies of what’s going on in the states, but those have faced additional complications, like rules that differ from state to state and an ongoing legalization of recreational use confusing the picture.
Just how confusing all this can be was driven home this week by the release of a paper that suggests that one of medical marijuana’s greatest successes was illusory. A couple of early studies indicated that states that had legalized medical marijuana use saw drops in opioid-related deaths. The new research replicates those results but finds that the trend has reversed in recent years, with those states now seeing increased deaths. While the new study’s authors suggest the initial results were spurious, others suggest that the shifting legal landscape and changes in drug abuse may have driven the change.
What does everyone agree upon?
Back in 2014, researchers compared deaths due to opioid abuse in states with and without legalization of medical marijuana. For the decade prior to 2010, the trend was clear: states that allowed medical marijuana had lower rates of opioid-abuse-driven death.
While this was a correlation study that couldn’t get at causal mechanisms, it wasn’t too difficult to find a plausible explanation: one of the uses of medical marijuana has been the management of severe pain, the same thing opioids are used to treat. Substitution of marijuana for these pain medications provides an obvious mechanism that could potentially explain the correlation. As later studies confirmed this trend, the finding ended up being used in the ongoing political debates about appropriate policies for marijuana use.
That set the stage for the new study, which uses the data from the earlier work but expands its scope to include the years up to and including 2017. Instead of a 20% drop, the study finds a 20% increase in opioid abuse deaths in states that have legalized medical marijuana.
Superficially, this may look like yet another case of a prominent study failing to replicate. In fact, the authors note that if they cut off the data at 2010, they are able to reproduce the earlier study’s results. It’s just that, starting around 2005, the trend in the correlation flattened out and then began rising sharply in about 2012. The changes prior to 2010 were too brief and mild to dramatically affect the trend found in the longer data set; those after 2012 were simply unavailable when the original study was conducted.
So, everyone is agreed that the original trend was real, and the analysis that revealed the most recent trend is scientifically sound. Where people are differing is in the interpretation.
A spurious connection?
So, what are the possibilities that could explain why a correlation would go away over time? The simplest explanation, and the one the new papers argue for, is that the correlation was spurious in the first place. Things happened to line up for a brief period but eventually diverged because they weren’t related in the first place.
The paper makes a number of arguments in favor of the connection being spurious. It notes that medical cannabis users are only 2.5 percent of the total population, raising questions as to whether they can have much of an effect on society-wide trends. But they also undercut that argument to a degree by noting that a separate study of medical cannabis found that its users were more likely to both use and abuse prescription painkillers. That suggests that medical cannabis has a better chance of influencing trends in the specific population at risk of opioid overdoses.
In the view of the paper’s authors, however, the association between medical marijuana use and painkiller abuse is inconsistent with the former limiting the latter. They add that there’s no obvious connection between the number of opioid overdose deaths and the stringency of marijuana laws, which can range from strict limits on the types of cannabis available for medicinal use to allowing recreational use. At the moment, however, the more extreme policies have only been in place for short periods of time and in a limited number of states, so analyzing them separately leads to enormous statistical uncertainty. As such, it’s really impossible to say anything about the effects of policy stringency yet.
But what else have we learned?
To get an additional perspective on this issue, we talked to one of the authors of the first paper that described the medical marijuana-opioid correlation. Chinazo Cunningham practices internal medicine, including addiction treatments, at the Albert Einstein College of Medicine. She argued that the original reasons for thinking that the correlation might be significant are still valid and have been supported by additional data in the meantime. “Randomized clinical trials show that cannabis reduces pain in people,” Cunningham told Ars. “And then we also have several studies that have shown that states that have medical cannabis have reduced opioid prescribing. We also know that patients report taking less opioids for their pain when they use cannabis.”
(While we were preparing this coverage, another paper was released showing that medical marijuana laws are associated with reduced opioid prescriptions. But it found that recreational marijuana laws are not, and the effects were specific to those younger than 55.)
While these don’t mean that the correlation was an indication of a real connection, Cunningham suggested that they are enough to make it worth considering. And, if there was a connection, this suggests something must have changed to decouple the two.
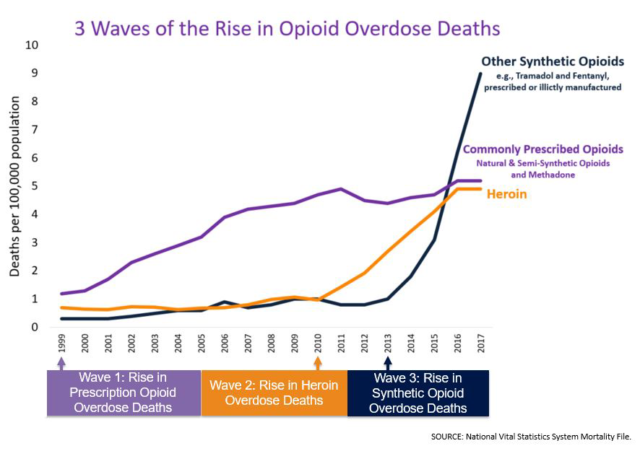
Cunningham had a couple of ideas about what might account for that change. One is a change in the cause of opioid overdose deaths. The rise in deaths from prescription opioids stabilized around 2010, the point where the original study ran out of data, and has been roughly flat since. By contrast, deaths due to heroin started climbing dramatically at about the same time, and that was followed by an even more rapid rise in deaths due to synthetic opioids like fentanyl, which began in 2015. It’s possible that the change in focus from prescription medications to illicit drugs, or the elevated potency of fentanyl, has altered the relationship with marijuana that’s supposed to be used for medical purposes.
Another potential confounding influence Cunningham noted was that there might have been a change in the populations involved because of the states that legalized medicinal cannabis since 2010. “We know that the states with the highest opioid overdose death rates, Ohio, West Virginia, and Pennsylvania, have all just recently legalized medical cannabis,” she said. This isn’t to say that the original correlation was definitely informative; it instead suggests that we shouldn’t discard the information as spurious without looking into these additional factors further.
But the possible factors that Cunningham mentions indicate that figuring anything out will be difficult. “There’s a host of other things that are happening at the same time [that changes in] the medical cannabis policies are also happening,” she said. While researchers are trying to track the changes happening in drug abuse, the drugs being abused are changing, the states that allow medicinal cannabis are changing, and the availability of cannabis is changing rapidly.
And Cunningham, like the authors of the new paper, highlights that all we can do right now is track correlation. “We need to do the studies that can determine causality—the randomized control trial. And in order to do that, the federal government has to change policy,” she told Ars, referring to the limits placed on studies of marijuana. “Until that happens, we’re all going to be guessing, or it’s going to be a little bit of a leap of faith while states are continuing to move forward. And really, that’s terrible. Our policies should be guided by science.”
PNAS, 2019. DOI: 10.1073/pnas.1903434116 (About DOIs).
https://arstechnica.com/?p=1521721

