While we have a number of treatments available for clinical depression, many of them have a significant side effects, and a lot of people struggle to find a drug that they respond to. The situation is made worse by our limited understanding of the biology underlying depression. We don’t know how to create targeted drugs, so most of the available treatments are blunt instruments that can take weeks to months before having an effect.
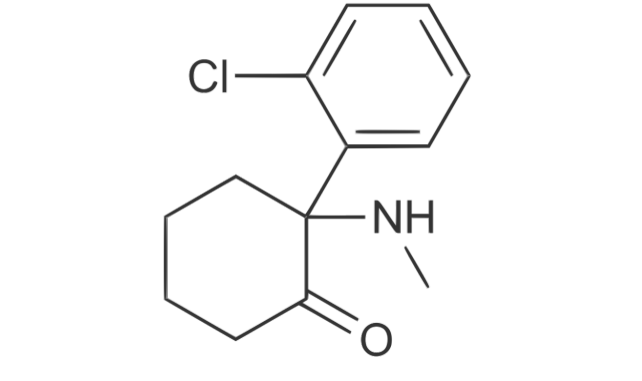
In that light, it came as a bit of a shock when we discovered a drug we’d been using recreationally and for anesthesia could lift the symptoms of depression in less than 24 hours. Unfortunately, the drug in question, ketamine, also has a collection of unpleasant side-effects, and we had no idea how it was working.
But there’s been significant progress in unravelling the confusion over ketamine, with researchers identifying a ketamine derivative that tackles depression with far fewer side effects. And this week, a team of researchers at China’s Zhejiang University announced that they’ve figured out where in the brain ketamine acts when it blocks depression, a finding that gives us significant insights into the biology of the disorder.
Ketamine and depression
The new studies rely on the work of a number of other labs, which have identified a specific structure deep in the brain that’s associated with depression. Called the lateral habenula, it’s been associated with a variety of activities, the most relevant of which seems to be the processing of unpleasant outcomes and punishment. Electrodes implanted there have been used to relieve depression in at least one instance.
To test whether this might be the site of ketamine’s activity, one team of researchers infused the drug directly into the lateral habenula of rats with depression-like symptoms; it blocked them. So did a separate chemical that inhibits the same proteins that ketamine acts on. Tracking the activity in the area, the researchers were able to show that there are bursts of activity in rats with symptoms of depression that are absent in healthy rats. The drugs that blocked depression suppressed these bursts.
To confirm that was really causal, the researchers performed the converse experiment, engineering cells in the lateral habenula to emit bursts of activity in response to light. This showed that the bursts themselves were enough to drive depressive symptoms in these animals.
A second paper, produced by many of the same researchers, describes what’s going on at the cellular level in the habenula. In this work the team induced depression in rats either chemically or by inducing what’s called “learned helplessness.” (The latter involves training the rats to recognize that they have no control over negative consequences in their environment.) The team then obtained tissue samples from the lateral habenula and examined every single protein produced there, looking for differences between depressed and healthy animals.
Ion flow
The most interesting result to come out of this was a protein that controls the flow of ions between a cell and its environment. That’s not much of a surprise, given that nerve impulses are driven by the exchange of ions across a nerve cell’s membrane. But the protein identified here isn’t made by nerve cells. Instead, it’s made by a type of cell called an astrocyte.
Astrocytes were once thought to be merely support cells that helped provide a good environment for nerve cells. But we’ve developed a significant body of evidence that hints that they may be involved in signaling with nerves as well.
In the case of depression, it doesn’t seem that direct signaling is involved. Instead, it’s involved in the process of resetting the nerve cell after an impulse, which requires gathering back all the ions that flowed out of the cell during the impulse. By changing the amount of potassium available to the nerve cell, the protein identified by this team alters the ease with which a nerve cell can fire again. By increasing the dose of this gene, the researchers were able to induce depression-like symptoms in mice; knocking the gene down reduced their ability to induce depressive behavior.
None of this is to say that this team has found a “cause of depression” or something similar. Depression is a complicated disorder, and it’s unlikely that there’s going to be a single underlying cause. What they have found, however, is something that’s likely to be central to the generation of the symptoms we associate with the disorder. Excess activity of a brain region thought to be involved in processing negative rewards makes a lot of sense as a trigger for the symptoms of depression, while the protein identified here makes sense as a trigger for this excess activity.
Just as critically, the work shows that drugs are able to disrupt this process. We’re still at the point where these drugs have significant side effects, but we now know a bit about what their targets are doing and where they have to act. That will hopefully lead to something a bit more specific before too long.
Nature, 2017. DOI: 10.1038/nature25509, 10.1038/nature25752 (About DOIs).
https://arstechnica.com/?p=1261721

