While cancerous cells look a lot like normal human cells, they’re still different enough that the immune system regularly attacks them. Obviously, this attack sometimes bogs down, allowing cancer to thrive and spread. Figuring out how to get the immune system back on track has been a major focus of research, and success in the area has been honored with a Nobel Prize.
Despite these successes, many patients aren’t helped by the newer immune-focused therapies, raising questions of what else we still need to figure out to help cancer patients. A new paper highlights something we may have missed: a class of immune cells that appears to be primed specifically to attack cancer. But the finding raises questions about what it is on cancer cells that the immune cells are recognizing and why they fail to keep cancer in check.
Finding cancer killers
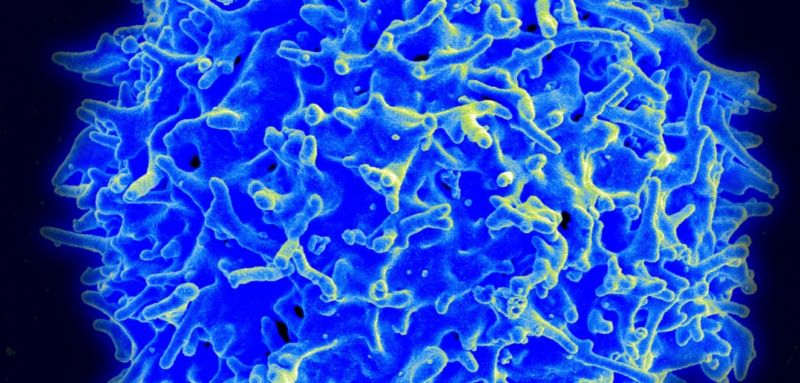
The start of this work was pretty simple: a large international team of researchers grew a mix of immune cells called “T cells” in the presence of cancerous cells and looked for cells that grew rapidly. This rapid growth is typically a sign that the immune cells have been activated by something they recognize—in this case, the cancer. They identified one particular lineage of T cells that grew well and named it MC.7.G5, confirming yet again that most scientists don’t belong in the creative industries.
One notable thing about the MC.7.G5 cells quickly became apparent: MC.7.G5 didn’t simply grow well in the presence of cancer cells; it killed them. So, the authors tested a variety of different cancer types (lung cancer, melanoma, colon, breast, and more). These cells don’t have much in common. They’re activated by different mutations, start out with different populations of proteins on their surface, and have many other differences from one another. So it wasn’t clear what the T cells could possibly be recognizing on their surfaces in order to attack them. Yet attack them they did.
To find out, the researchers did an experiment that wouldn’t have been possible just a decade earlier: they used a gene-editing construct to eliminate every single protein-coding gene that we know of in the genome. Lots of individual populations of a cancer-cell line had a single gene knocked out and then were tested to see whether the MC.7.G5 immune cells could still kill them. If any cancer cells were left alive, then the gene edited in them would be essential for producing the molecule used by the immune cells to recognize cancer.
The experiment identified a series of genes involved in putting a single protein on the surface. But, of course, that protein is also present on normal cells. How could it possibly be responsible for the cancer cells being recognized as distinct?
Fortunately, we know a lot about the family of molecules that the protein, MR1, belongs to, as well as a bit about MR1 itself. The larger family includes the molecules that help the immune system recognize self from non-self by binding to bits of the cell’s proteins and presenting them on the cell’s surface for the immune system to check out. If either these molecules or the proteins they present look different, the immune system attacks. So, that makes a degree of sense as something that can trigger the immune system to go after the cancer cells.
MR1, however, doesn’t work like that. Instead, it brings some of the cell’s metabolites to the surface. And the researchers confirmed that it has to bind to something in order to make it to the surface. They hypothesize that it’s a metabolite that’s specific to cancer cells, but they have no idea what it might be.
Stay on target
While there are still some question marks about what causes these immune cells to pick out cancerous cells, there’s no shortage of evidence that they do so effectively. The researchers tested the immune cells against resting and dividing normal cells and got no response. MC.7.G5 didn’t kill healthy cells that were stressed or damaged. So, there’s no indication that the immune cells accidentally go off target and kill healthy cells.
The researchers also confirmed that the cancer-killing T cells are defined by the standard receptor that T cells normally use to recognize infected cells. They made a copy of this receptor’s genes and inserted them into T cells from an unrelated individual. They also killed cancerous cells from at least two different sources.
Finally, the authors injected lymphoma cells into immune-compromised mice, then added the cancer-killing T cells. In control mice without the cancer-killing cells, the lymphoma took over the bone marrow, eventually accounting for about 80 percent of the cells there. With the cancer-killing cells injected at the same time, the bone marrow in the mice consistently had far fewer cancer cells (consistently less than 10 percent of the total cells). This indicates that the immune cells can help keep cancer in check but may not be able to consistently eradicate it.
Does that mean, as the BBC has claimed, that these cells “May treat all cancer”? Well, to begin with, the T cells were seemingly unable to eliminate cancer in mice. That’s more significant than it seems, in that lots of potential treatments seem to work well in mice, but few ever advance to the point of clinical trials in humans, much less end up being used as treatments. This is a case when mouse assays are helpful for knowing what deserves a closer look but far from the last word on a topic.
Do we all have cancer killers?
These cancer-killing immune cells were also obtained from at least two individuals, suggesting that they may be present in all humans. Yet humans regularly suffer from cancer, so there’s clearly something that keeps them from doing their job. At this point, we don’t have the slightest clue as to what that something might be.
Then there’s the issue of what the cells are recognizing that allows them to identify cancer cells. Whatever it is, it’s not widely present on healthy cells. But the body has a dizzying number of specialized cell types, so we’ve barely scratched the surface of testing whether these cells might attack some healthy cell types. However, if the authors are right about a couple of things, there’s a very good chance the cells might.
The authors suggest that the target of the cancer-killing cells is a metabolite presented on the surface by the protein MR1. And, because the gene-editing screen didn’t pull out any metabolic enzymes, they suspect that the metabolite is essential for cancer cell viability. It’s difficult to understand how something central to cancer cell viability, produced using the same genes found in normal cells, isn’t ever produced by normal cells.
None of this is to say that this discovery won’t end up being important. But we really need much more information before we’re in a position to judge whether it is or not.
Nature Immunology, 2020. DOI: 10.1038/s41590-019-0578-8 (About DOIs).
https://arstechnica.com/?p=1647381

