On Monday, a press release from the transnational pharmaceutical company Pfizer dropped a rare spark of hope into the ongoing misery of the COVID-19 pandemic. Yes, new infections have hit an all-time high in the United States, and, yes, cities and states around the world are walking back their reopenings. But Pfizer says it has results from a massive clinical trial showing that its vaccine against the disease works, and works well. The release touted “a vaccine efficacy rate above 90 percent,” and it announced the company’s intention to seek from the US Food and Drug Administration an authorization to start giving people shots. The company’s ready to make 50 million doses this year and 1.3 billion doses in 2021.
That’s an ember of hope, but it’s sitting under a bucket of cold water, ready to pour. The Pfizer vaccine is finicky—hard to make, transport, and deliver. Because of desperate need, it’s in short supply even before it becomes available—1.3 billion doses is several billion short of what the world needs. The press release wasn’t peer-reviewed science, and it lacked critical details about how the vaccine works and on whom. Even the simple fact of this vaccine’s existence, some analysts have argued, might jeopardize the testing and success of potentially better vaccines down the line, a case of the imperfect being the enemy of the good.
Before the ember dies out completely, here’s a theory: no. The Pfizer vaccine’s imperfections make it a perfect prime mover, because if it works as well as the company says, it’ll help people now and require research into more, better, different vaccines for later. All the things nobody knows about the Pfizer vaccine mean that the door is wide open. “Whether its effects are durable, whether it’s effective in the elderly, whether it has safety issues, the cold chain issues, the ability to have access,” says Wayne Koff, president and CEO of the nonprofit Human Vaccines Project, “all that points to the need for a number of vaccines.”

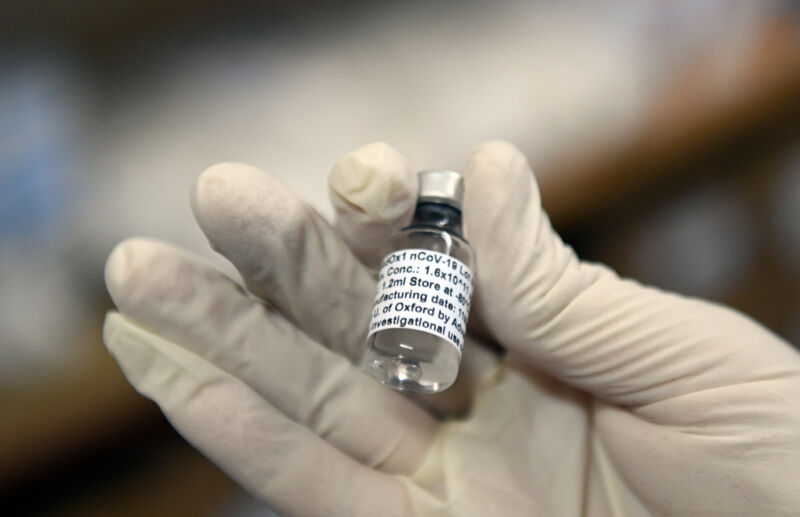
Working with a smaller company called BioNTech, Pfizer moved off the starting block fast, and without the money from the US Operation Warp Speed program that funded other drug companies’ trials. This vaccine (like another candidate made by the company Moderna) is actually a tailored bit of genetic material called messenger RNA; give it to people, and the mRNA acts like biological software, teaching cells to manufacture the “spike” protein on the outer coat of the virus that causes COVID-19. Those people’s immune systems then learn to recognize and attack the spike, which gives them the ability to fight the virus. It’s a cool idea, and as my colleague Megan Molteni has written, it could change the future of vaccinology and infectious disease.
Cold case
But this is the first mRNA vaccine, and it turns out to be a precious little snowflake. Pfizer’s vaccine has to be stored and shipped at ultracold temperatures, less than 80 degrees below zero—it’ll keep for a few days at higher but still very cold conditions. And it needs vials made of a special glass that’s able to tolerate the freezing temperatures. (This is neat, actually—the key is that the glass is low in boron, exactly the opposite of famously temperature-change-tolerant Pyrex glass, which is a mix of boron and silicon dioxide. The glassmaker Corning has a $204 million contract with the government to make it and cut a deal in May to provide it to Pfizer. Whether Corning can make enough is the tricky part.)
All that shipping and freezing requires a level of technical sophistication that, for now at least, mostly exists in hospitals and labs—posing significant logistical challenges in rural areas and in the developing world. These are the “cold chain” problems that Koff mentioned, the problem of refrigerated shipping. (A critical Ebola vaccine needs the same deep freeze, and engineers stepped up to create specialized coolers to transport it across western Africa—but that was a pandemic that affected tens of thousands of people, not billions, and the people who made the coolers have since gotten out of the cold-chain innovation game.)
“Minus 70 is almost a nonstarter”
Those logistical challenges and an overall shortage of the vaccine are going to limit even further who gets the vaccine first. A spokesperson for Pfizer says the company has built its own network of distribution centers, freezers, and specialized shipping containers. And, meanwhile, Phase I of any vaccination plan will probably involve giving it to health care workers and first responders—the kind of people who’ll have easier access to the places that actually have the drug, and are perhaps more likely to come back for the second shot the Pfizer vaccine requires.
“We understand that Pfizer has a network of locations that it worked with to conduct its clinical trials throughout the United States,” says Anna Legried Dopp, senior director for clinical guidelines and quality improvement at the American Society of Health-System Pharmacists. Dopp says she understands there to be upwards of 100 of these locations. “They’ll leverage the ultracold freezers that were given to them for purposes of the clinical trial,” she says.
This is good; the freezers will be able to change temperatures to accommodate other, future, vaccine candidates that need cold, but not as cold, conditions (like, apparently, Moderna’s).
OK. So at least one set of weaknesses might also be a strength. So might some others. “We’ll probably figure out how to solve, in the short term, the cold chain, just because the estimates of the economic costs I’ve seen in the US are in the trillions of dollars. Longer term, in the US and globally, something that has to be at minus 70 is almost a nonstarter,” says Sam Scarpino, a mathematical epidemiologist at Northeastern University who studies disease spread. “We’ll continue to find out more and more about the vaccine as it scales up from Phase III to being injected in 100 million people, and then a billion people—whether it turns out that there are other things we need out of a vaccine, and if other stuff remains in the pipeline.”
Science by press release
What Scarpino means is, the Pfizer vaccine might be good enough to start healing the world but not good enough to finish the job. Pfizer has promised a peer-reviewed, detailed accounting of results, but for now it’s just a press release, and it leaves a lot out. (Getting science by press release is never ideal.) Pfizer and the FDA withstood extraordinary political pressure to forgo faster-moving data releases that wouldn’t encompass potential side effects, yet the press release didn’t say anything about whether the vaccine shows different levels of protection in different demographic groups (most saliently children, adults, and the elderly) or has longer-term safety issues.
How could it? The vaccine is too new, and studying vaccine efficacy in subgroups is notoriously difficult. But policymakers are going to need that data, because they’re going to have to decide how to deploy limited supplies. If they know one vaccine is better for older people, that helps tell them where to send it—and vaccines will certainly have different skill sets.
https://arstechnica.com/?p=1723217

